- Research article
- Open access
- Published:
Can quality improvement improve the quality of care? A systematic review of reported effects and methodological rigor in plan-do-study-act projects
BMC Health Services Research volume 19, Article number: 683 (2019)
Abstract
Background
The Plan-Do-Study-Act (PDSA) method is widely used in quality improvement (QI) strategies. However, previous studies have indicated that methodological problems are frequent in PDSA-based QI projects. Furthermore, it has been difficult to establish an association between the use of PDSA and improvements in clinical practices and patient outcomes. The aim of this systematic review was to examine whether recently published PDSA-based QI projects show self-reported effects and are conducted according to key features of the method.
Methods
A systematic literature search was performed in the PubMed, Embase and CINAHL databases. QI projects using PDSA published in peer-reviewed journals in 2015 and 2016 were included. Projects were assessed to determine the reported effects and the use of the following key methodological features; iterative cyclic method, continuous data collection, small-scale testing and use of a theoretical rationale.
Results
Of the 120 QI projects included, almost all reported improvement (98%). However, only 32 (27%) described a specific, quantitative aim and reached it. A total of 72 projects (60%) documented PDSA cycles sufficiently for inclusion in a full analysis of key features. Of these only three (4%) adhered to all four key methodological features.
Conclusion
Even though a majority of the QI projects reported improvements, the widespread challenges with low adherence to key methodological features in the individual projects pose a challenge for the legitimacy of PDSA-based QI. This review indicates that there is a continued need for improvement in quality improvement methodology.
Background
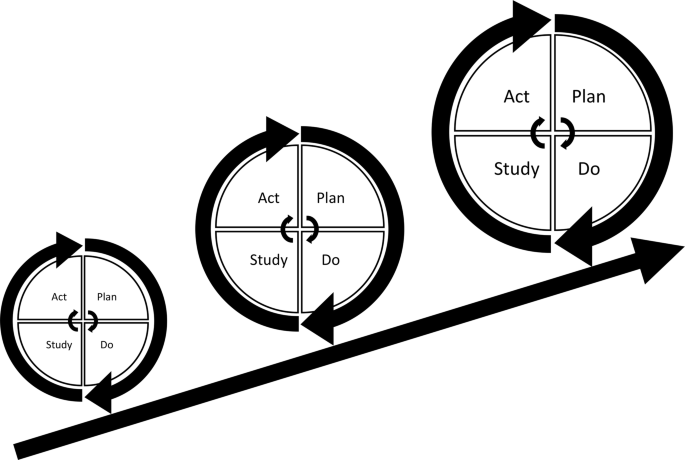
Plan-Do-Study-Act (PDSA) cycles are widely used for quality improvement (QI) in most healthcare systems where tools and models inspired by industrial management have become influential [1]. The essence of the PDSA cycle is to structure the process of improvement in accordance with the scientific method of experimental learning [2,3,4,5]. It is used with consecutive iterations of the cycle constituting a framework for continuous learning through testing of changes [6,7,8,9,10].
The concept of improvement through iterative cycles has formed the basis for numerous structured QI approaches including Total Quality Management, Continuous Quality Improvement, Lean, Six Sigma and the Model for Improvement [4, 6, 10]. These “PDSA models” have different approaches but essentially consist of improvement cycles as the cornerstone combined with a bundle of features from the management literature. Especially within healthcare, several PDSA models have been proposed for QI adding other methodological features to the basic principles of iterative PDSA cycles. Key methodological features include the use of continuous data collection [2, 6, 8,9,10,11,12,13], small-scale testing [6, 8, 10, 11, 14,15,16] and use of a theoretical rationale [5, 9, 17,18,19,20,21,22]. Most projects are initiated in the complex social context of daily clinical work [12, 23]. In these settings, focus on use of these key methodological features ensures quality and consistency by supporting adaptation of the project to the specific context and minimizing the risk of introducing harmful or wasteful unintended consequences [10]. Thus, the PDSA cycle is not sufficient as a standalone method [4] and integration of the full bundle of key features is often simply referred to as the PDSA method (Fig. 1).
Since its introduction to healthcare in the 1990s, numerous QI projects have been based on the PDSA method [10, 24]. However, the scientific literature indicates that the evidence for effect is limited [10, 25,26,27,28,29,30]. The majority of the published PDSA projects have been hampered with severe design limitations, insufficient data analysis and incomplete reporting [12, 31]. A 2013 systematic review revealed that only 2/73 projects reporting use of the PDSA cycle applied the PDSA method in accordance with the methodological recommendations [10]. These methodological limitations have led to an increased awareness of the need for more methodological rigor when conducting and reporting PDSA-based projects [4, 10]. This challenge is addressed by the emergent field of Improvement Science (IS) which attempts to systematically examine methods and factors that best facilitate QI by drawing on a range of academic disciplines and encourage rigorous use of scientific methods [5, 12, 32, 33]. It is important to make a distinction between local QI projects, where the primary goal is to secure a change, and IS, where the primary goal is directed at evaluation and scientific advancement [12].
In order to improve local QI projects, Standards for Quality Improvement Reporting Excellence (SQUIRE) guidelines have been developed to provide a framework for reporting QI projects [18, 34]. Still, it remains unclear to what extent the increasing methodological awareness is reflected in PDSA-based QI projects published in recent years. Therefore, we performed a systematic review of recent peer-reviewed publications reporting QI projects using the PDSA methodology in healthcare and focused on the use of key features in the design and on the reported effects of the projects.
Methods
The key features of PDSA-based QI projects were identified, and a simple but comprehensive framework was constructed. The review was conducted in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [35].
The framework
Informed by recommendations for key features in use and support of PDSA from literature specific to QI in healthcare the following key features were identified:
Aiming for conceptual simplicity, we established basic minimum requirements for the presence of the key features operationalizing them into binary (yes/no) variables. General characteristics and supplementary data that elaborated the use of the key features were operationalized and registered as categorical variables. See Table 1 for an overview of the framework and Additional file 1 for a more in-depth elaboration of the definitions used for the key features. Since a theoretical rationale can take multiple forms, the definition for this feature was taken from the recent version of the SQUIRE guidelines [18].
Since no formal standardized requirements for reporting PDSA-based QI projects across journals are established, not all report the individual PDSA cycles in detail. To ensure that variation in use of key features were inherent in the conduct of the projects and not just due to differences in the reporting, sufficient documentation of PDSA cycles was set as a requirement for analysis against the full framework.
Self-reported effects
A pre-specified, quantitative aim can assist to facilitate evaluation of whether the changes represent clinically relevant improvements when using the PDSA method [16]. Self-reported effects of the projects were registered using four categories: 1) Quantitative aim set and reached; 2) No quantitative aim set, improvement registered; 3) Quantitative aim set but not reached; 4) No quantitative aim and no improvement registered.
Systematic review of the literature
The target of the literature search was peer-reviewed publications that applied the PDSA cycle as the main method for a QI project in a healthcare setting. The search consisted of the terms ([‘PDSA’ OR ‘plan-do-study-act’] AND [‘quality’ OR ‘improvement’]). The terms were searched for in title and abstract. No relevant MeSH terms were available. To get a contemporary status of the QI field, the search was limited to QI projects published in 2015 and 2016. PubMed, Embase and CINAHL databases were searched with the last search date being 2nd of March 2017.
Study selection
The following inclusion criteria were used: Peer-reviewed publications reporting QI projects using the PDSA methodology in healthcare, published in English. Exclusion criteria were: IS studies, editorials, conference abstracts, opinions and audit articles, reviews or projects solely involving teaching the PDSA method.
Two reviewers (SVK and HVBL) performed the screening process independently. Title and abstract were screened for inclusion followed by an assessment of the full text according to the eligibility criteria. This was performed in a standardized manner with the Covidence software. Disagreements were resolved by consensus.
Data collection process
A data collection sheet was developed and pilot tested. The subsequent refinement resulted in a standardized sheet into which data were extracted independently by SVK and HVBL.
Data items
Data from the key and supplementary features were extracted in accordance with the framework. The binary data were used to grade QI projects on a scale of 0–4, based on how many of the four key features were applied. Data were analyzed in STATA (version 15.0, StataCorp LLC).
Results
Study selection
Selection process
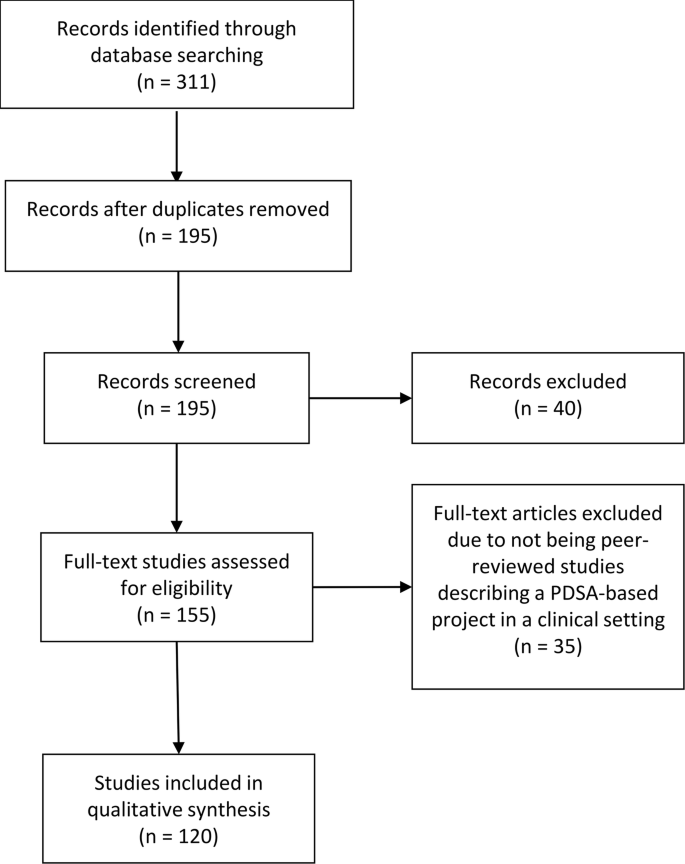
The search identified 311 QI projects of which 195 remained after duplicate removal. A total of 40 and 35 projects were discarded after screening abstracts and full texts, respectively. Hence, a total of 120 projects met the inclusion criteria and were included in the review (see Fig. 2).
An overview of general characteristics, supplementary features and self-reported effects of the included projects are presented in Table 2.
General characteristics
Country and journal
The included QI projects originated from 18 different countries including the USA (n = 52), the UK (n = 43), Canada (n = 6), Singapore (n = 5), Saudi Arabia (n = 4), Australia (n = 2) and one each from eight other countries. Fifty different journals had published QI projects with the vast majority (n = 53) being from BMJ Quality Improvement Reports. See Additional file 2 for a full summery of the findings.
Area and specialty
In terms of reach, most were local (n = 103) followed by regional (n = 13) and nationwide (n = 3). The areas of healthcare were primarily at departmental (n = 68) and hospital level (n = 36). Many different specialties were represented, the most common being pediatrics (n = 28), intensive or emergency care (n = 13), surgery (n = 12), psychiatry (n = 11) and internal medicine (n = 10).
Supporting framework
Most QI projects did not state using a supporting framework (n = 70). However, when stated, most used The Model for Improvement (n = 40). The last (n = 10) used Lean, Six-sigma or other frameworks.
Reported effects
All 120 projects included were assessed for the self-reported effects. Overall, 118/120 (98%) projects reported improvement. Thirty-two (27%) achieved a pre-specified aim set in the planning process, whereas 68 (57%) reported an improvement without a pre-specified aim. Eighteen projects (15%) reported setting an aim and not reaching it while two (2%) projects did not report a pre-specified aim and did not report any improvement.
Documentation
Seventy-two projects had sufficient documentation of the PDSA cycles. Sixty of these contained information on individual stages of cycles, while 12 in addition presented detailed information on the four stages of the PDSA cycles.
Application of key features of PDSA
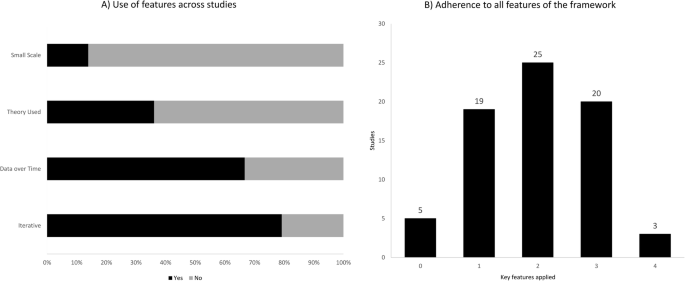
The application of the key PDSA features appeared to be highly inconsistent. The iterative method was used in 75 projects (79%), continuous data collection in 48 (67%), an explicit theoretical rational was present in 26 (36%) projects and small-scale testing was carried out by 10 (14%) (Fig. 3a). All key features of the method were applied in 3/72 projects (4%), while 20 (28%), 26 (36%), and 18 (25%) used three, two, and one feature respectively. Five projects (7%) lacked all features (Fig. 3b). See Additional file 3 for a full summary of the findings.
Iterative cycles
Fifty-seven projects (79%) had a sequence of cycles where one informed the actions of the next. A single iterative chain of cycles was used in 41 (57%), while four (5%) had multiple isolated iterative chains and 12 (17%) had a mix of iterative chains and isolated cycles. Of the 15 projects using non-iterative cycles, two reported a single cycle while 13 used multiple isolated cycles. The majority (55/72) (76%) tested one change per cycle.
Small scale testing
The testing of changes in a small scale was carried out by 10 projects (14%), of which seven did so in an increasing scale, while two kept testing at the same scale. It was unclear which type of scaling was used in the remaining project. Sixty-two projects (86%) carried out testing on an entire department or engaged in full-scale implementation before having tested the improvement intervention.
Continuous data collection
Continuous measurements over time with three or more data points at regular intervals were used by 48 (67%) out of 72 projects. Of these 48, half used run charts, while the other half used control charts. Other types of data measurement such as before and after or per PDSA cycle or having a single data point as outcome after cycle(s) was done by 18 (25%) and 5 (7%), respectively. One project did not report their data. Sixty-five projects (90%) used a baseline measurement for comparison.
Theoretical rationale
Twenty-six (36%) out of 72 projects explicitly stated the theoretical rationale of the project describing why it was predicted to lead to improvement in their specific clinical context. In terms of inspiration for the need for improvement 68 projects (94%) referred to scientific literature. For the QI interventions used in the projects 26 (36%) found inspiration in externally existing knowledge in forms of scientific literature, previous QI projects or benchmarking. Twenty-one (29%) developed the projects themselves, 10 (14%) used existing knowledge in combination with own ideas while 15 (21%) did not state the source.
Discussion
In this systematic review nearly all PDSA-based QI projects reported improvements. However, only approximately one out of four projects had defined a specific quantitative aim and reached it. In addition, only a small minority of the projects reported to have adhered to all four key features recommended in the literature to ensure the quality and adaptability of a QI project.
The claim that PDSA leads to improvement should be interpreted with caution. The methodological limitations in many of the projects makes it difficult to draw firm conclusions about the size and the causality of the reported improvements in quality of care. The methodological limitations question the legitimacy of PDSA as an effective improvement method in health care. The widespread lack of theoretical rationale and continuous data collection in the projects makes it difficult to track and correct the process as well as to relate an improvement to the use of the method [10, 11]. The apparent limited use of the iterative approach and small-scale-testing constitute an additional methodological limitation. Without these tools of testing and adapting one can risk introducing unintended consequences [1, 36]. Hence, QI initiatives may potentially tamper with the system in unforeseen ways creating more harm and waste than improvement. The low use of small-scale-testing could perhaps originate in a widespread misunderstanding that one should test large-scale to get a proper statistical power. However, this is not necessarily the case with PDSA [15].
There is no simple answer to this lack of adherence to the key methodological features. Some scholars claim that even though the concept of PDSA is relatively simple it is difficult to master in reality [4]. Some explanations to this have been offered including an urge to favour action over evidence [36], an inherent messiness in the actual use of the method [11], its inability to address “big and hairy” problems [37], an oversimplification of the method, and an underestimation of the required resources and support needed to conduct a PDSA-based project [4].
In some cases, it seems reasonable that the lack of adherence to the methodological recommendations is a problem with documentation rather than methodological rigor, e.g. the frequent lack of small-scale pilot testing may be due to the authors considering the information too irrelevant, while still having performed it in the projects.
Regarding our framework one could argue that it has too many or too few key features to encompass the PDSA method. The same can be said about the supplementary features where additional features could also have been assessed e.g. the use of Specific, Measurable, Attainable, Relevant and Timebound (SMART) goals [14]. It has been important for us to operationalize the key features so their presence easily and accurately can be identified. Simplification carries the risk of loss of information but can be outweighed by a clear and applicable framework.
This review has some limitations. We only included PDSA projects reported in peer-reviewed journals, which represents just a fraction of all QI projects being conducted around the globe. Further, it might be difficult to publish projects that do not document improvements. This may introduce potential publication bias. Future studies could use the framework to examine the grey literature of evaluation reports etc. to see if the pattern of methodological limitations is consistent. The fact that a majority of the projects reported positive change could also indicate a potential bias. For busy QI practitioners the process of translating a clinical project into a publication could well be motivated by a positive finding with projects with negative effects not being reported. However, we should not forget that negative outcome of a PDSA project may still contribute with valuable learning and competence building [4, 6].
The field of IS and collaboration between practitioners and scholars has the potential to deliver crucial insight into the complex process of QI, including the difficulties with replicating projects with promising effect [5, 12, 20, 32]. Rigorous methodological adherence may be experienced as a restriction on practitioners, which could discourage engagement in QI initiatives. However, by strengthening the use of the key features and improving documentation the PDSA projects will be more likely to contribute to IS, including reliable meta-analyses and systematic reviews [10]. This could in return provide QI practitioners with evidence-based knowledge [5, 38]. In this way rigor in performing and documenting QI projects benefits the whole QI community in the long run. It is important that new knowledge becomes readily available and application oriented, in order for practitioners to be motivated to use it. An inherent part of using the PDSA method consists of acknowledging the complexity of creating lasting improvement. Here the scientific ideals about planning, executing, hypothesizing, data managing and documenting with rigor and high quality should serve as inspiration.
Our framework could imply that the presence of all four features will inevitably result in the success of an improvement project. This it clearly not the case. No “magic bullets” exist in QI [39]. QI is about implementing complex projects in complex social contexts. Here adherence to the key methodological recommendations and rigorous documentation can help to ensure better quality and reproducibility. This review can serve as a reminder of these features and how rigor in the individual QI projects can assist the work of IS, which in return can offer new insight for the benefit of practitioners.
Conclusion
This systematic review documents that substantial methodological challenges remain when reporting from PDSA projects. These challenges pose a problem for the legitimacy of the method. Individual improvement projects should strive to contribute to a scientific foundation for QI by conducting and documenting with a higher rigor. There seems to be a need for methodological improvement when conducting and reporting from QI initiatives.
Availability of data and materials
All data generated or analysed during this review are included in this published article and its supplementary information files.
Abbreviations
- IS:
-
Improvement Science
- PDSA:
-
Plan-Do-Study-Act
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QI:
-
Quality Improvement
- SMART:
-
Specific, Measurable, Attainable, Relevant and Timebound
- SQUIRE:
-
Standards for QUality Improvement Reporting Excellence
References
Nicolay CR, Purkayastha S, Greenhalgh A, Benn J, Chaturvedi S, Phillips N, et al. Systematic review of the application of quality improvement methodologies from the manufacturing industry to surgical healthcare. Br J Surg. 2012;99(3):324–35.
Speroff T, O’Connor GT. Study designs for PDSA quality improvement research. Qual Manag Health Care. 2004;13(1):17–32.
Moen R. Foundation and history of the PDSA cycle. Assoc Process Improv. 2009; Available from: https://deming.org/uploads/paper/PDSA_History_Ron_Moen.pdf.
Reed JE, Card AJ. The problem with plan-do-study-act cycles. BMJ Qual Saf. 2016;25(3):147–52.
Portela MC, Lima SML, Martins M, Travassos C. Improvement Science: conceptual and theoretical foundations for its application to healthcare quality improvement. Cad Saude Publica. 2016;32(sup 2):e00105815.
Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide, 2nd edition. Jossey-Bass. 2009.
Berwick DM. The science of improvement. JAMA - J Am Med Assoc. 2008;299(10):1182–4.
Berwick DM, Nolan TW. Developing and testing changes in delivery of care. Ann Intern Med. 1998;128(1):651–6.
Perla RJ, Provost LP, Parry GJ. Seven propositions of the science of improvement: exploring foundations. Qual Manag Health Care. 2013;22(3):170–86.
Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf 2013;0:1–9.
Ogrinc G. Building knowledge, asking questions. BMJ Qual Saf. 2014;23(4):265–7.
Portela MC, Pronovost PJ, Woodcock T, Carter P, Dixon-Woods M. How to study improvement interventions: a brief overview of possible study types. Postgrad Med J. 2015;91(1076):343–54.
Thor J, Lundberg J, Ask J, Olsson J, Carli C, Härenstam KP, et al. Application of statistical process control in healthcare improvement: systematic review. Qual Saf Heal Care. 2007;16(5):387–99.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50.
Etchells E, Ho M, Shojania KG. Value of small sample sizes in rapid-cycle quality improvement projects. BMJ Qual Saf. 2016;25(3):202–6.
Berwick DM. A primer on leading the improvement of systems. BMJ Br Med J. 1996;312(7031):619.
Speroff T, James BC, Nelson EC, Headrick LA, Brommels M. Guidelines for appraisal and publication of PDSA quality improvement. Qual Manag Health Care. 2004;13(1):33–9.
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. Standards for QUality Improvement Reporting Excellence 2.0: revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25:986–92.
Moonesinghe SR, Peden CJ. Theory and context: putting the science into improvement. Br J Anaesth. 2017;118(4):482–4.
Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf. 2015;24(3):228–38.
Foy R, Ovretveit J, Shekelle PG, Pronovost PJ, Taylor SL, Dy S, et al. The role of theory in research to develop and evaluate the implementation of patient safety practices. BMJ Qual Saf. 2011;20(5):453–9.
Walshe K. Pseudoinnovation: the development and spread of healthcare quality improvement methodologies. Int J Qual Heal Care. 2009;21(3):153–9.
Walshe K. Understanding what works-and why-in quality improvement: the need for theory-driven evaluation. Int J Qual Heal Care. 2007;19(2):57–9.
Powell AE, Rushmer RK, Davies HT. A systematic narrative review of quality improvement models in health care. Glasgow: Quality Improvement Scotland (NHS QIS ). 2009.
Groene O. Does quality improvement face a legitimacy crisis? Poor quality studies, small effects. J Heal Serv Res Policy. 2011;16(3):131–2.
Dixon-Woods M, Martin G. Does quality improvement improve quality? Futur Hosp J. 2016;3(3):191–4.
Blumenthal D, Kilo CM. A report Card on continuous quality improvement. Milbank Q. 1998;76(4):625–48.
Dellifraine JL, Langabeer JR, Nembhard IM. Assessing the evidence of six sigma and lean in the health care industry. Qual Manag Health Care. 2010;19(3):211–25.
D’Andreamatteo A, Ianni L, Lega F, Sargiacomo M. Lean in healthcare: a comprehensive review. Health Policy (New York). 2015;119(9):1197–209.
Moraros J, Lemstra M, Nwankwo C. Lean interventions in healthcare: do they actually work? A systematic literature review. Int J Qual Heal Care. 2016:150–65.
Shojania KG, Grimshaw JM. Evidence-based quality improvement: the state of the science. Health Aff. 2005;24(1):138–50.
Marshall M, Pronovost P, Dixon-Woods M. Promotion of improvement as a science. Lancet. 2013;381(9881):419–21.
The Health Foundation. Improvement science. Heal Found Heal Scan. 2011. Available from: http://www.health.org.uk/sites/health/files/ImprovementScience.pdf.
Davidoff F, Batalden P, Stevens D, Ogrinc G, Mooney S. Publication guidelines for quality improvement in health care: evolution of the SQUIRE project. Qual Saf Heal Care. 2008;17(SUPPL. 1):i3–9.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. BMJ Br Med J. 2009;339:b2700.
Auerbach AD, Landefeld CS, Shojania KG. The tension between needing to improve care and knowing how to do it. N Engl J Med. 2007;357(6):608–13.
Dixon-Woods M, Martin G, Tarrant C, Bion J, Goeschel C, Pronovost P, et al. Safer clinical systems: evaluation findings. Heal Found. 2014; Available from: https://www.health.org.uk/publications/safer-clinical-systems-evaluation-findings.
Dixon-Woods M, Bosk CL, Aveling EL, Goeschel CA, Pronovost PJ. Explaining Michigan: developing an ex post theory of a quality improvement program. Milbank Q. 2011;89(2):167–205.
Oxman AD, Thomson MA, Davis DA, Haynes B. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. Cmaj. 1995;153(10):1423–31.
Acknowledgements
Not applicable.
Funding
The review was funded by Aalborg University, Denmark. The funding body had no influence on the study design, on the collection, analysis and interpretation of data or on the design of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors have made substantive intellectual contributions to the review. SVK and HVBL have been the primary authors and have made substantial contributions to conception and design, acquisition, analysis and interpretation of the data as well as developing drafts of the manuscript. LHE and JM have been primary supervisors and have contributed substantially with intellectual feedback and manuscript revision. SPJ and PB have made substantial contributions by revising the manuscript critically for intellectual content. Each author agrees to be accountable for all aspects of the work and all authors have given final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Description of variables and coding. (DOCX 24 kb)
Additional file 2:
Projects identified in the search that used PDSA method. (DOCX 204 kb)
Additional file 3:
Projects identified in search that describes PDSA method in sufficient detail to be included for full analysis for framework. (DOCX 145 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Knudsen, S.V., Laursen, H.V.B., Johnsen, S.P. et al. Can quality improvement improve the quality of care? A systematic review of reported effects and methodological rigor in plan-do-study-act projects. BMC Health Serv Res 19, 683 (2019). https://doi.org/10.1186/s12913-019-4482-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-019-4482-6