- Research
- Open access
- Published:
Exploring patients’ perspectives: a mixed methods study on Outpatient Parenteral Antimicrobial Therapy (OPAT) experiences
BMC Health Services Research volume 24, Article number: 544 (2024)
Abstract
Background
Outpatient Parenteral Antimicrobial Therapy (OPAT), an alternative to inpatient intravenous antibiotic therapy, has shown benefits in international studies such as increased patient satisfaction. Because OPAT has been used only sporadically in Germany so far, no structured results on patients’ experiences and concerns regarding OPAT have yet been available. This study therefore aims to explore the experiences of OPAT patients in a pilot region in Germany.
Methods
This is an observational study in a German pilot region, including a survey of 58 patients on their experiences with OPAT, and in-depth interviews with 12 patients (explanatory-sequential mixed-methods design).
Results
Patients reported that they were satisfied with OPAT. That a hospital discharge was possible and anti-infective therapy could be continued in the home environment was rated as being particularly positive. In the beginning, many patients in the interviews were unsure about being able to administer the antibiotic therapy at home on their own. However, healthcare providers (doctors and pharmacy service provider staff) were able to allay these concerns. Patients appreciated regular contact with care providers. There were suggestions for improvement, particularly concerning the organization of the weekly check-up appointments and the provision of information about OPAT.
Conclusions
Patients were generally satisfied with OPAT. However, the treatment structures in Germany still need to be expanded to ensure comprehensive and high-quality OPAT care.
Trial registration
NCT04002453, https://www.clinicaltrials.gov/, (registration date: 2019–06-21).
Background
When hospitalisation is required solely to administer intravenous antibiotic therapy to treat an infectious disease, Outpatient Parenteral Antimicrobial Therapy (OPAT) offers a means to entirely circumvent hospitalisation or at least significantly reduce its duration [1, 2]. OPAT involves the delivery of approved parenteral antibiotic therapy outside of an inpatient hospital setting. Typically, a secure vascular catheter is inserted, allowing for the administration of the anti-infective therapy via infusion. OPAT can be carried out in various settings, including a general practitioner’s office, a specialised outpatient facility, or even the patient's own home [2]. Patients may self-administer or receive assistance from an informal caregiver or professional caregiver [2, 3]. Typical indications for OPAT include skin and soft tissue infection, bone infection, and endocarditis, which are often associated with the need for prolonged intravenous antibiotic therapy [2, 4]. Offering comparable efficacy to inpatient care, OPAT presents numerous advantages, including a lower risk of nosocomial infections [5, 6]. At the same time, costs can be saved by preventing or shortening hospital stays [4, 7,8,9]. OPAT is therefore an efficacious and safe alternative to inpatient treatment [10, 11]. Research on OPAT consistently underscores the high levels of patient satisfaction attributable to its seamless integration into their daily routines [8, 12,13,14,15,16]. OPAT is a standard care practice in many countries [3, 17, 18]. However, in Germany, there is a lack of healthcare infrastructure, regulations, and recommendations to support OPAT [1]. As a result, OPAT is only offered by few specialised centres or practices [2, 19]. There has been little research about patients’ experiences with OPAT in Germany, despite the fundamental and active role of patients in this mode of treatment. In the spirit of patient-centred outcome measurement, this article aims to answer the question: How is OPAT experienced and accepted by patients in an urban pilot region of Germany (Cologne metropolitan region)? In a nationwide comparison, Cologne has an advantage in the developement of an OPAT structures: an infectiological network (consisting, for example, of hospitals and outpatient infectiological practices) dedicated to patient care, education and training and also research, e.g. for OPAT [1].
Methods
A prospective observational study as part of the K-APAT study (“outpatient parenteral antibiotic treatment in the metropolitan region of Cologne”), which scientifically evaluated the implementation of OPAT in a German pilot region (the Cologne metropolitan region), was conducted. Clinical data is published separately [20]. A detailed description of the study design can be found in the study protocol [21]. The study has been approved by the Institutional Review Board of the University of Cologne, Germany (19–1284-1). The study is a multi-centre study consisting of 5 hospitals and 5 outpatient practices with a focus on infectiology. All study centres were allowed to include patients in the study [21]. Patients who were considered suitable for OPAT by the infectious disease service were also enrolled in the patient satisfaction survey study after giving informed consent to OPAT. Inclusion criteria were therefore admission as an OPAT patient; a minimum age of 18 years; and written informed consent to the survey study. As the survey documents could only be provided in German, sufficient knowledge of German was mandatory. Data collection was carried out using an explanatory mixed-methods design between November 2019 and September 2021 [22]. The explanatory mixed-methods design allows a broad yet thorough understanding of the patient perspective [22]. Patients were invited to answer up to three surveys delivered by mail about their OPAT experience at three timepoints: T0 (before starting OPAT, 48 items), T1 (two weeks after starting OPAT, 51 items) and T2 (one week after finishing OPAT, 42 items). Most of the items were likert scaled. All questionnaires included one open ended question (“If you have any comments, please note them here:”). After the patients were enrolled in the study, a written questionnaire was sent to their homes if they had given their consent. The data was collected pseudonymously in returning the questionnaire to the research institute, which was not involved in the treatment of the patients. The questionnaires were developed based on the current literature [2, 11, 13, 23,24,25,26,27,28,29] and critically reviewed by the study team consisting of social scientists, healthcare researchers, and clinicians with expertise in infectious diseases. The questionnaires used in the K-APAT study were developed specifically for this research. A German version is available in the project's final report [30]. Both self-developed questions and validated instruments were used in the questionnaires. The final report also contains information on validated and self-developed items [30]. The questionnaires were tested for comprehensibility and adapted within the framework of ten cognitive pretests with healthy adult persons of different age groups (19 to 70 years old). Topics of the questionnaires are shown in Table 1 (Tab. 1). See the appendix for the English version of the questionnaire items used for this publication (Additional file 1). Data were analysed descriptively using Stata 17 software.
After the quantitative data collection, in-depth interviews were conducted with selected patients who answered the questionnaires beforehand. These patients had indicated in the written declaration of consent for the study that they would be interested in taking part in in-depth interviews once the questionnaire survey had been completed. The patients were selected for the interviews by the researchers using the pseudonymised data set. The researchers were not involved in the patients' medical care and were only familiar with the patients’ T0, T1 and T2 questionnaires. The researchers wanted to map the greatest possible variability of the patients, especially with regard to their experiences and satisfaction with OPAT. Patients were also selected for a balance in gender, age, duration of OPAT treatment, and overall satisfaction with OPAT. All 12 interviews took place in person (mostly at patients' homes) or by telephone, due to contact restrictions during the COVID-19 pandemic.
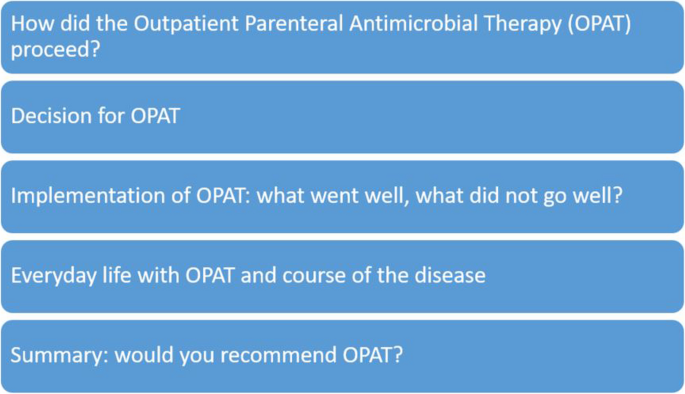
Topics of the interview guide are shown in Fig. 1 (Fig. 1). The English version of the interview guide is available as a Supplementary file (Additional file 2). Dimensions of the semi-structured interview guide were developed from the literature [11, 23,24,25,26,27,28,29] and expert feedback. The interview guide utilised in the K-APAT study was specifically developed for this research. The German version can be found in the final report [30].
The qualitative data were interpreted by means of a content analysis (inductive and deductive categories), which was carried out iteratively by SP and CO [31].
The participants received a financial incentive for completing the questionnaires and participating in the interviews.
Results
Patients’ characteristics can be found in Table 2 (Tab. 2).
As stated in the publication on the projects’ clinical data, the most frequently treated infections were joint and bone infections (26% of the patients) and vertebral osteomyelitis (14% of the patients) [20]. All results (including the overall results of the three questionnaires and the interviews) and all items of the survey instruments are included in the final report of the K-APAT project [30].
Results from the questionnaires
All 77 patients included in the study returned their questionnaires (response rate: 100%). 19 respondents did not answer at least one item of the questionnaire which are reported here. These patients were therefore excluded from the following analyses.
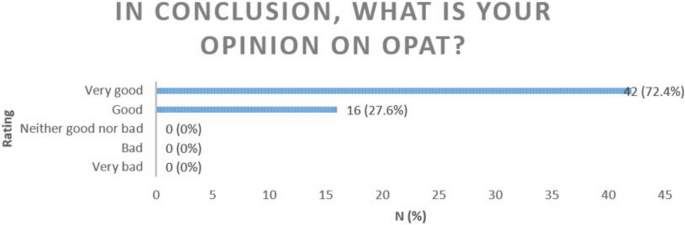
In the first and second questionnaire (T0 and T1) patients were asked about their experiences with OPAT subdivided in e.g. therapy confidence, experiences with intravenous antbiotic therapy and patient education (all topics are summarised in Table 1). In T2, all patients were asked to summarise their OPAT treatment. The aim was to obtain a final evaluation of their entire OPAT treatment. All respondents had a positive opinion on OPAT (Fig. 2).
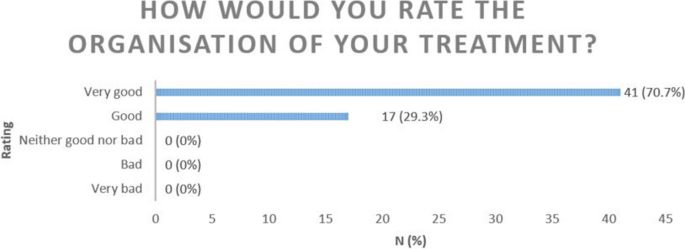
Also as part of the final conclusion to their OPAT most patients rated the organisation of their treatment as good (29.3%) or very good (70.7%) (Fig. 3).
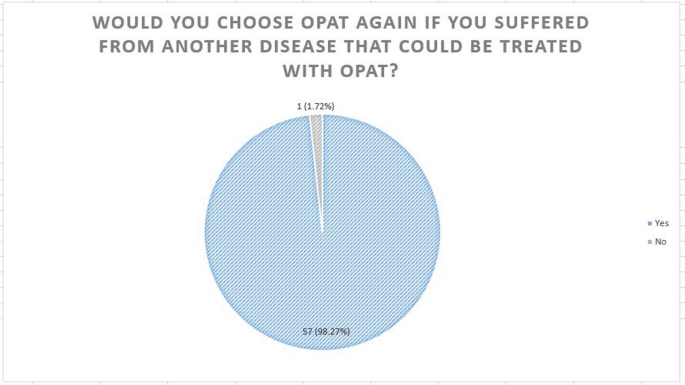
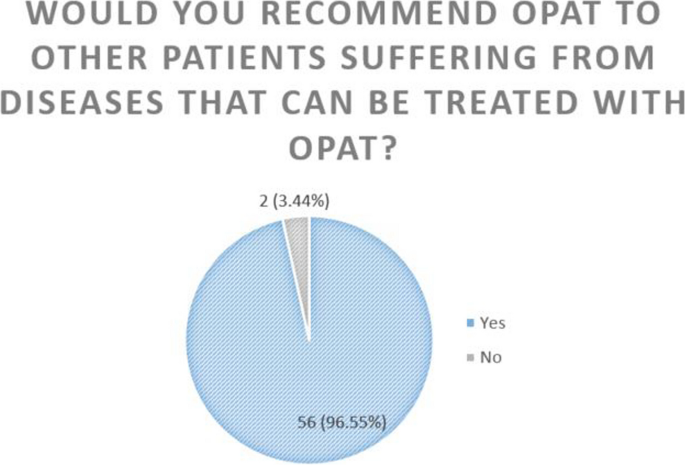
The majority of patients (98.28%) would choose OPAT again if required. A similarly high proportion (96.55%) would recommend OPAT (Figs. 4 & 5).
Patients were asked to indicate their problems with OPAT using a Likert scale (strongly disagree, rather disagree, rather agree, strongly agree): Problems with material storage were infrequently reported, with only 10.34% strongly agreeing and 3.45% rather agreeing. A small number of individuals (1.72% strongly agree, 8.62% rather agree) reported feeling uncomfortable with the vascular catheter, while 13.9% tended to agree that the vascular catheter affected how they were perceived in public. Additionally, 12.07% strongly agreed and 18.97% rather agreed that they deliberately hid their vascular catheter in public. Eight people (3.45% strongly agree, 10.34% rather agree) reported complications during their treatment. None of the respondents reported any mistakes made by the medical staff, or that OPAT was an inappropriate treatment option for them (Table 3).
Results from the interviews
The results of the interviews are summarised in the Table 4 (Tab. 4).
The interviews lasted between 20 and 58 min (mean length: 39 min).
Despite the overall positive evaluation of OPAT, some difficulties were identified during the interviews following explicit enquiries. Eight of the interviewees reported anxiety or uncertainty, especially at the beginning of their therapy (e.g., fear of making mistakes when administering antibiotics; fear of venous catheter management because of the “at heart” location). One patient commented: “This [OPAT] is excellent. Painless and great. However, it is a strange feeling considering the access is in the heart [sic]. (…) You do have a queasy feeling. (…) But it is great. I always thought: Well, what if it slips? But how is it supposed to slip? Slipping is not possible.” (patient 4). However, most fears quickly subsided after the start of therapy. One patient reported severe mechanical problems due to blockage of the catheter, which led to her being switched to oral medication for the last 3 days of her treatment: "Overall it went well and only few problems occurred. Sometimes it happened that, [patient paused and reformulated] So once I had difficulty taking it [the pump system] off again. We then had to use a pipe wrench.” (patient 8). However, most patients had no problems with the OPAT at all. One interviewee said: “And, yes, here at home I had no problems at all. Even the first application, I did it a bit more carefully, of course, just to not forget anything, to do everything right, and very quickly routine comes in.” (patient 5). Another patient summarised: “There were no problems of any kind. There was no pain. There were no incidents.” (patient 9). Motor and cognitive limitations were mentioned as possible barriers to handling infusions.
The interviewees reported numerous benefits of the OPAT. They could be discharged from the hospital early, which they associated with greater self-determination and higher quality of life than in the hospital. One patient stated: “So that [the OPAT] has already given me a lot of freedom.” (patient 11) and another patient mentioned: “As I said, I’m at home, I have my familiar surroundings, and then I feel like I’m back to a normal life and I have the disease under control. So it [the OPAT] was a good way to not have to keep going back to the doctor again and again.” (patient 6). All interviewees emphasised how important it was for their well-being to be at home. One patient explained: “That I can be at home. That’s important for me because I feel most comfortable at home. I have 100 TV channels, and at the hospital, I have five that I don’t really watch at home. Or I can eat whatever I feel like. Home is home.” (patient 7). Freedom and independence in a homecare setting were highly valued compared to the lack of freedom and dependence in inpatient care. A lot of patients explained that OPAT at home was easy to perform and helpful for recovery. In addition, the treatment was predictable: “That was ritualised. I then took a book at some point and read, sat down in the corner and read. I didn't move wildly, right?” (patient 3). Patients did not feel that OPAT interfered with their daily life. In the words of one interviewee:”So everything I do here at home, I’ve been able to do with the [venous catheter].” (patient 10). One patient added: “I would say top-notch. I can only recommend it to everyone. So who is fit enough: definitely. Yes. Although I was also in the hospital [patient paused and started a new sentence] They were all super nice, doctors, nurses, everyone. They really did their best, but home is home, right? And if you really have the opportunity, (…) immediately. So I would do that again immediately. Yes. I hope not that I need it again, but let’s just say I would do it in a heartbeat.” (patient 12). In addition, three patients who work in healthcare themselves stated that OPAT is associated with cost savings for the healthcare system. They emphasised that no hospitalisation or nursing service is required for this treatment. From their experience, the venous catheter can stay in place for longer and does not need to be constantly replaced compared to peripheral catheters, and they heal well.
The interviewees reported some restrictions in everyday life due to OPAT: e.g., sleeping on the side with the catheter is uncomfortable, financial challenges (e.g., co-payment for those with statutory insurance was not explained and cost coverage for those with private insurance was initially unclear, both should be communicated more clearly), insecurity in handling, and suspected side effects (e.g., fatigue, eczema, exhaustion that patients attributed to their OPAT) were also reported by the patients. Most patients did not describe any side effects: “And I didn’t have any side effects or anything. So not that I felt anything bad, that I felt bad, that I felt dizzy or anything. It went wonderfully.” (patient 1).
The interviewees also reported their experiences with healthcare providers. Often patients mentioned a lack of awareness of OPAT among healthcare providers in the hospital and organisational barriers such as waiting times. The venous catheter placement and removal took place in the hospital for all patients. Weekly check-ups were also primarily performed in a hospital outpatient clinic. One patient reported on her hospital stay as: “I already noticed that the doctor was a bit worried […] and then [he] told me to make sure that I observe the hygiene measures, that would be very important. I think there is a bit of fear when you hand things over to the patient: let's see what the patient does with it himself? Surely there are differences there, right?” (patient 8). The interviewed patients evaluated the support by the pharmacy service providers as well-organised. The deliveries of the material (e.g. bandages, material for cleaning catheters, disinfectant) were organised well and without problems. The study participants received a high quantity of material, often more than was required. The OPAT briefing was good and adapted to the patients' needs. Nevertheless, the interviewees reported that the information they got from their healthcare providers was partially incomprehensible (e.g. the step-by-step instruction of the OPAT is very complex with preparation of the material, cleaning of the skin and the catheter and connecting the pumps). One patient felt that she had generally received too little information about OPAT from her physicians. The patients liked the check-ups and the option to contact the healthcare providers by phone: “Yes, she [the pharmacy employee] also called me again herself, I think on the fourth day, which I thought was very nice, and asked if everything was okay, if I was getting along, if I needed anything else.” (patient 2). Outpatient providers such as General Practitioners and other outpatient care services played a minor role among respondents and were only sporadically involved in treatment. Overall, the patients rated the organisation of the OPAT as good.
Discussion
Main findings
In the K-APAT study, a prospective observational study, we aimed to investigate medical care with OPAT, focusing on the model region of Cologne. The goal was to assess the feasibility and success of implementing OPAT within the German healthcare system. The sub-study we presented here aimed to find out more about patient views on OPAT, their satisfaction, and their experience within the framework of a mixed-methods study.
In our study, OPAT had high levels of patient satisfaction, with nearly all patients expressing contentment. Other studies found comparable satisfaction with OPAT treatment with similar rates of recommendation and reporting that they would opt for OPAT again if necessary [13, 26]. Saillen et al. (2017) concluded that OPAT patients were “happy to take over some responsibility for their treatment” [26]. In general, patient satisfaction with OPAT is comparably high internationally [8, 12,13,14,15,16]. Quintens et al. (2020) also reported that all respondents were very satisfied with their OPAT treatment [32]. However, some patients in their study as well as in Berrevoets et al. (2018) also wanted more information about the OPAT and reported side effects attibuted to the OPAT [11, 32] as the patients in our interviews did too. Similarly as can be seen in our data, Saillen et al. (2017) reported that patients initially had concerns about the self-application of and reported on mechanical problems in handling the pump system [26].
Notably, the most satisfying aspect was that this form of treatment allowed patients to be discharged from the hospital. This effect does not only apply to the OPAT patients reported here: As hospitalisation is often perceived as a burden [33, 34], a lot of patients express satisfaction upon discharge from the hospital. The organisation of OPAT was largely perceived to be good. In particular, patients appreciated regular contact with healthcare providers (physicians and pharmacy service providers). It is important for the success of the therapy that patients feel comfortable and well cared for [11].
In countries where OPAT is well established, the number of patients participating in OPAT studies is significantly higher [35]. One Italian study showed that the COVID-19 pandemic supported the use of OPAT [10]. The number of participants in our study fell during the pandemic. We suspect that this is due to the heavy burden on hospital staff and outpatient practices.
Strengths and limitations
It is important to consider limitations when interpreting the results of this study. It was conducted in the densely populated metropolitan region of Cologne: the findings may therefore not be fully representative of other regions in Germany (e.g. rural areas, regions without infectiological networks). But the region was well suited to conducting a feasibility study on OPAT due to the already established expertise of the regional, infectiological network. In addition, most of the study was conducted during the COVID-19 pandemic, which could have led to a number of limitations. For example, our participant number (N = 58) is low. Although all 77 patients we included in the study returned their questionnaires (response rate: 100%), due to missing values, we had to remove 19 patients from the dataset. We attempted to improve recruitment by having multiple study sites and conducting the study in a region that has a good OPAT care structure by national standards. Nevertheless, the case number limits the generalisability of the data. However, other international studies have reported similarly low participation rates [32, 36,37,38].
Compared to other studies our patient population was mostly younger (mean of survey patients: 55.2 years) except for the study presented by Al Shareef et al. (2022) with the same median age as in our study [38]: Chambers et al. (2019) reported on patients with a median age of 61 years [35]. Saillen et al. (2017), Staples et al. (2022) and Berrevoets et al. (2018) also reported a higher median age of 59 years, 62 years and even 68 years [11, 14, 26]. Treatment periods in our population (survey data: mean: 15 days, interview data: mean: 27 days) were higher than in other studies. Wolter et al. (2004) reported about 11 days, Hase et al. (2020) reported 13 days and Saillen et al. (2017) 8.5.days [8, 26, 36]. As is common in many other OPAT studies, our survey data also has a high proportion of male participants. [11, 14, 32, 36, 38].
It is particularly interesting that in the survey, OPAT was described as good or very good. More detailed insights from the interviews showed that, despite the overall good rating, patients had minor problems with OPAT. Thus, the mixed-methods design and the extensive interview data complement the quantitative data well, e.g. patients were able to report on their experiences in more detail and more individually than it was possible in the questionnaires. Thus, the mixed-methods design supported the breadth and depth of data [39] on patients' OPAT experiences.
We tried to include a wide range of patient experiences with OPAT in the in-depth interviews and have made efforts to achieve a gender and age balance of the interviewees. But as you can see in Table 2 the interviewees were a little older and had a longer treatment period of OPAT compared to the survey population. In addition, the proportion of men in the survey was higher than in the interviews. Despricption on the underlying diseases can be found in the publication on the clinical data [20]. Unfortunately, patients who would not recommend OPAT (N = 2) to others or tended to be less satisfied than average either did not consent to be contacted for an interview or were unwilling to be interviewed when asked to do so.
A professional proofreading service performed proofreading of this publication.
Implications
In the long term, OPAT can be a suitable option for standard care.
OPAT not only increases patient satisfaction through cross-sector, indication-based and patient-oriented care, but also relieves the burden on hospitals by reducing inpatient bed days [1]. Moreover, the inpatient sector is facing mounting pressures arising from a scarcity of specialists, demographic shifts, and soaring costs. In response, healthcare policy is advocating for the expansion of the outpatient care model, guided by the principle of “outpatient care before inpatient care” [40].
The data has shown that the OPAT programme can be improved in the following ways to further increase patient satisfaction: Some patients reported they did not know about potential co-payments, which should be communicated more clearly. Waiting times for check-ups in hospitals or doctors' offices should also be reduced. Patients have expressed the wish for flyers or information material explaining the OPAT procedure as well as the handling of the intravenous access in more detail. This improvement has already been introduced into care at the study sites: Flyers and videos describing the OPAT procedure have been developed.
Conclusions
This study shows a high level of patient satisfaction with OPAT. The preference for home-based treatment over hospital care is a key contributing factor. OPAT is still a relatively uncommon procedure in Germany, which is why there are still no nationwide structures for this treatment option. However, our studie shows that patients are satisfied with the care they received and that an expansion of the OPAT structures should therefore be considered. In the studied region, a quality infrastructure for OPAT exists, marked by specialists in specialised and interconnected outpatient clinics. Due to all of these advantages, it is important to further promote the use of OPAT and broaden these prerequisites by establishing adequate OPAT structures [41].
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- K-APAT:
-
Outpatient parenteral antibiotic treatment in the metropolitan region of Cologne
- OPAT:
-
Outpatient Parenteral Antimicrobial Therapy
References
Terhalle E, Jung N, Stegemann MS, Priesner V, Lehmann C, Schmiedel S. Neue Entwicklungen in der ambulanten parenteralen Antibiotikatherapie (APAT). [New developments in outpatient parenteral antibiotic therapy (OPAT)]. Dtsch Med Wochenschr. 2020;145:1688–94. https://doi.org/10.1055/a-1114-3990.
Stegemann M, Hagel S, Lehmann C. Antibiotikatherapie (2): Ambulante parenterale Gabe. Deutsches Ärzteblatt Online. 2019. https://doi.org/10.3238/PersInfek.2019.07.22.03.
Norris AH, Shrestha NK, Allison GM, Keller SC, Bhavan KP, Zurlo JJ, et al. 2018 infectious diseases society of America clinical practice guideline for the management of outpatient parenteral antimicrobial therapy. Clin Infect Dis. 2019;68:e1–35. https://doi.org/10.1093/cid/ciy745.
Petrak RM, Skorodin NC, Fliegelman RM, Hines DW, Chundi VV, Harting BP. Value and clinical impact of an infectious disease-supervised outpatient parenteral antibiotic therapy program. Open Forum Infect Dis. 2016;3:ofw193. https://doi.org/10.1093/ofid/ofw193.
Rentala M, Andrews S, Tiberio A, Alagappan K, Tavdy T, Sheppard P, Silverman R. Intravenous home infusion therapy instituted from a 24-hour clinical decision unit for patients with cellulitis. Am J Emerg Med. 2016;34:1273–5. https://doi.org/10.1016/j.ajem.2016.04.022.
Kayley J, Berendt AR, Snelling MJ, Moore H, Hamilton HC, Peto TE, et al. Safe intravenous antibiotic therapy at home: experience of a UK based programme. J Antimicrob Chemother. 1996;37:1023–9. https://doi.org/10.1093/jac/37.5.1023.
Dalovisio JR, Juneau J, Baumgarten K, Kateiva J. Financial impact of a home intravenous antibiotic program on a medicare managed care program. Clin Infect Dis. 2000;30:639–42. https://doi.org/10.1086/313755.
Wolter JM, Cagney RA, McCormack JG. A randomized trial of home vs hospital intravenous antibiotic therapy in adults with infectious diseases. J Infect. 2004;48:263–8. https://doi.org/10.1016/S0163-4453(03)00135-X.
Dimitrova M, Gilchrist M, Seaton RA. Outpatient parenteral antimicrobial therapy (OPAT) versus inpatient care in the UK: a health economic assessment for six key diagnoses. BMJ Open. 2021;11:e049733. https://doi.org/10.1136/bmjopen-2021-049733
Giuliano G, Raffaelli F, Faliero D, Tamburrini E, Tarantino D, Nurchis MC, Scoppettuolo G. Outpatient parenteral antimicrobial therapy (OPAT) from an emergency model applied during the COVID-19 pandemic to standard of care: preliminary lessons from our experience. Infect Dis Now. 2023;53;104642. https://doi.org/10.1016/j.idnow.2023.01.002
Berrevoets MAH, Oerlemans AJM, Tromp M, Kullberg BJ, ten Oever J, Schouten JA, Hulscher ME. Quality of outpatient parenteral antimicrobial therapy (OPAT) care from the patient’s perspective: a qualitative study. BMJ Open. 2018;8: e024564. https://doi.org/10.1136/bmjopen-2018-024564.
Wong KK, Fraser TG, Shrestha NK, Fatica C, Deshpande A. Low incidence of Clostridium difficile infection (CDI) in patients treated with outpatient parenteral antimicrobial therapy (OPAT). Infect Control Hosp Epidemiol. 2015;36:110–2. https://doi.org/10.1017/ice.2014.6.
MacKenzie M, Rae N, Nathwani D. Outcomes from global adult outpatient parenteral antimicrobial therapy programmes: a review of the last decade. Int J Antimicrob Agents. 2014;43:7–16. https://doi.org/10.1016/j.ijantimicag.2013.09.006.
Staples JA, Ho M, Ferris D, Hayek J, Liu G, Tran KC, Sutherland JM. Outpatient Versus Inpatient Intravenous Antimicrobial Therapy: A Population-Based Observational Cohort Study of Adverse Events and Costs. Clin Infect Dis. 2022;75:1921–9. https://doi.org/10.1093/cid/ciac298.
Board N, Brennan N, Caplan GA. A randomised controlled trial of the costs of hospital as compared with hospital in the home for acute medical patients. Aust N Z J Public Health. 2000;24:305–11. https://doi.org/10.1111/j.1467-842x.2000.tb01573.x.
Corwin P, Toop L, McGeoch G, Than M, Wynn-Thomas S, Wells JE, et al. Randomised controlled trial of intravenous antibiotic treatment for cellulitis at home compared with hospital. BMJ. 2005;330:129. https://doi.org/10.1136/bmj.38309.447975.EB.
Chapman ALN, Seaton RA, Cooper MA, Hedderwick S, Goodall V, Reed C, et al. Good practice recommendations for outpatient parenteral antimicrobial therapy (OPAT) in adults in the UK: a consensus statement. J Antimicrob Chemother. 2012;67:1053–62. https://doi.org/10.1093/jac/dks003.
Hatcher J, Costelloe C, Cele R, Viljanen A, Samarasinghe D, Satta G, et al. Factors associated with successful completion of outpatient parenteral antibiotic therapy (OPAT): A 10-year review from a large West London service. Int J Antimicrob Agents. 2019;54:207–14. https://doi.org/10.1016/j.ijantimicag.2019.04.008.
Rieg S, Küpper MF. Infectious diseases consultations can make the difference: a brief review and a plea for more infectious diseases specialists in Germany. Infection. 2016;44:159–66. https://doi.org/10.1007/s15010-016-0883-1.
Schmidt-Hellerau K, Baade N, Günther M, Scholten N, Lindemann CH, Leisse C, et al. Outpatient parenteral antimicrobial therapy (OPAT) in Germany: insights and clinical outcomes from the K-APAT cohort study. Infection. 2024. https://doi.org/10.1007/s15010-024-02199-9.
Scholten N, Leisse C, Brandes V, Oberröhrmann C, Ihle P, Peter S, et al. Outpatient parenteral antimicrobial therapy in Germany: a prospective cohort study protocol. BMJ Open. 2022;12:e061417. https://doi.org/10.1136/bmjopen-2022-061417.
Cresswell JW. A concise introduction to mixed methods research. 2nd ed. Thousand Oaks, CA: SAGE Publications; 2022.
Ansari AA. Outpatient Parenteral Antimicrobial Therapy (OPAT) in the Kingdom of Bahrain: Efficacy. Patient Satisfaction and Cost Effectiveness TOIDJ. 2013;7:90–5. https://doi.org/10.2174/1874279301307010090.
Baecker H, Gessmann J, Hanusrichter Y, Zahn PK, Schildhauer TA, Frieler S. Die ambulante i. v. Antibiotikatherapie mittels PICC Line in der Behandlung von chronischen periprothetischen Infektionen. [Outpatient Parenteral Antibiotic Therapy (OPAT) with Peripherally Inserted Central Catheter in Patients with Periprosthetic Joint Infection]. Z Orthop Unfall. 2019;157:510–4. https://doi.org/10.1055/a-0830-4776.
Esposito S, Noviello S, Leone S, Tice A, Seibold G, Nathwani D, Scaglione F. Outpatient parenteral antibiotic therapy (OPAT) in different countries: a comparison. Int J Antimicrob Agents. 2004;24:473–8. https://doi.org/10.1016/j.ijantimicag.2004.06.004.
Saillen L, Arensdorff L, Moulin E, Voumard R, Cochet C, Boillat-Blanco N, et al. Patient satisfaction in an outpatient parenteral antimicrobial therapy (OPAT) unit practising predominantly self-administration of antibiotics with elastomeric pumps. Eur J Clin Microbiol Infect Dis. 2017;36:1387–92. https://doi.org/10.1007/s10096-017-2944-5.
Townsend J, Keller S, Tibuakuu M, Thakker S, Webster B, Siegel M, et al. Outpatient parenteral therapy for complicated Staphylococcus aureus infections: a snapshot of processes and outcomes in the real world. Open Forum Infect Dis. 2018;5:ofy274. https://doi.org/10.1093/ofid/ofy274.
Twiddy M, Czoski Murray CJ, Mason SJ, Meads D, Wright JM, Mitchell ED, Minton J. A qualitative study of patients’ feedback about Outpatient Parenteral Antimicrobial Therapy (OPAT) services in Northern England: implications for service improvement. BMJ Open. 2018;8:e019099. https://doi.org/10.1136/bmjopen-2017-019099
Gardiol C, de Vallière S. Ambulante parenterale Antibiotikatherapie: Aktuelle Empfehlungen für die parenterale Behandlung von Infektionen. Swiss Medical Forum - Schweizerisches Medizin-Forum. 2016;16:314–8.
Lehmann C, Leisse C, Lindemann C, Scholten N, Oberröhrmann C, Ihle P, et al. Ergebnisbericht: Ambulante parenterale Antibiotikatherapie in der Kölner Metropolregion (K-APAT). 2023. https://innovationsfonds.g-ba.de/downloads/beschluss-dokumente/436/2023-08-16_K-APAT_Ergebnisbericht.pdf. Accessed 26 Mar 2024.
Kuckartz U. Qualitative Inhaltsanalyse: Methoden, Praxis, Computerunterstützung. 4th ed. Weinheim: Beltz Verlagsgruppe; 2018.
Quintens C, Steffens E, Jacobs K, Schuermans A, van Eldere J, Lagrou K, et al. Efficacy and safety of a Belgian tertiary care outpatient parenteral antimicrobial therapy (OPAT) program. Infection. 2020;48:357–66. https://doi.org/10.1007/s15010-020-01398-4.
Gonçalves-Bradley DC, Lannin NA, Clemson L, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev. 2022;2:CD000313.
Mäkelä P, Stott D, Godfrey M, Ellis G, Schiff R, Shepperd S. The work of older people and their informal caregivers in managing an acute health event in a hospital at home or hospital inpatient setting. Age Ageing. 2020;49:856–64. https://doi.org/10.1093/ageing/afaa085.
Chambers ST, Basevi A, Gallagher K, Carswell-Moyna A, Isenman H, Pithie A, et al. Outpatient parenteral antimicrobial therapy (OPAT) in Christchurch: 18 years on. N Z Med J. 2019;132:21–32.
Hase R, Yokoyama Y, Suzuki H, Uno S, Mikawa T, Suzuki D, et al. Review of the first comprehensive outpatient parenteral antimicrobial therapy program in a tertiary care hospital in Japan. Int J Infect Dis. 2020;95:210–5. https://doi.org/10.1016/j.ijid.2020.03.033.
Kwok CS, Whittaker JJ, Malbon C, White B, Snape J, Lloyd V, et al. Outpatient parenteral antimicrobial therapy (OPAT) service is associated with inpatient-bed cost savings. Br J Cardiol. 2021;28:38. https://doi.org/10.5837/bjc.2021.038.
Al Shareef HJ, Al Harbi A, Alatawi Y, Aljabri A, Al-Ghanmi MA, Alzahrani MS, et al. Evaluate the Effectiveness of Outpatient Parenteral Antimicrobial Therapy (OPAT) Program in Saudi Arabia: A Retrospective Study. Antibiotics (Basel). 2022. https://doi.org/10.3390/antibiotics11040441.
Schoonenboom J, Johnson RB. How to Construct a Mixed Methods Research Design. Kolner Z Soz Sozpsychol. 2017;69:107–31. https://doi.org/10.1007/s11577-017-0454-1.
Bundesministerium für Justiz. Sozialgesetzbuch (SGB) Fünftes Buch (V) - Gesetzliche Krankenversicherung - § 39 Krankenhausbehandlung; 1988. https://www.gesetze-im-internet.de/sgb_5/__39.html. Accessed 26 Mar 2024.
Chapman ALN, Patel S, Horner C, Gilchrist M, Seaton RA. Outpatient parenteral antimicrobial therapy: updated recommendations from the UK. J Antimicrob Chemother. 2019;74:3125–7. https://doi.org/10.1093/jac/dkz343.
Acknowledgements
We would like to thank all patients who participated in our study. We would also like to thank all of the staff at the study centres and the pharmacy service providers who cared for the patients together with the study physicians.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the German Federal Joined Committee (grant number 01VSF18036).
Author information
Authors and Affiliations
Contributions
ClL led the K-APAT study. NS, CO and SP designed the questionnaires and the interview guide, and have mainly carried out and evaluated the data collection. SP wrote the first draft of the manuscript. AH, ChL, ClL, CO, HP, JKN, KSH, NS, PI and VB substantively revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the Institutional Review Board of the University of Cologne, Germany (19-1284-1). Participants signed a written consent form to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peter, S., Oberröhrmann, C., Pfaff, H. et al. Exploring patients’ perspectives: a mixed methods study on Outpatient Parenteral Antimicrobial Therapy (OPAT) experiences. BMC Health Serv Res 24, 544 (2024). https://doi.org/10.1186/s12913-024-11017-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11017-9