- Research
- Open access
- Published:
On-demand mobile hypertension training for primary health care workers in Nigeria: a pilot study
BMC Health Services Research volume 24, Article number: 444 (2024)
Abstract
Background
Only one out of every ten Nigerian adults with hypertension has their blood pressure controlled. Health worker training is essential to improve hypertension diagnosis and treatment. In-person training has limitations that mobile, on-demand training might address. This pilot study evaluated a self-paced, case-based, mobile-optimized online training to diagnose and manage hypertension for Nigerian health workers.
Methods
Twelve hypertension training modules were developed, based on World Health Organization and Nigerian guidelines. After review by local academic and government partners, the course was piloted by Nigerian health workers at government-owned primary health centers. Primary care physician, nurse, and community health worker participants completed the course on their own smartphones. Before and after the course, hypertension knowledge was evaluated with multiple-choice questions. Learners provided feedback by responding to questions on a Likert scale.
Results
Out of 748 users who sampled the course, 574 enrolled, of whom 431 (75%) completed the course. The average pre-test score of completers was 65.4%, which increased to 78.2% on the post-test (P < 0.001, paired t-test). Health workers who were not part of existing hypertension control programs had lower pre-test scores and larger score gains. Most participants (96.1%) agreed that the training was applicable to their work, and nearly all (99.8%) agreed that they enjoyed the training.
Conclusions
An on-demand mobile digital hypertension training increases knowledge of hypertension management among Nigerian health workers. If offered at scale, such courses can be a tool to build health workforce capacity through initial and refresher training on current clinical guidelines in hypertension and other chronic diseases in Nigeria as well as other countries.
Background
Hypertension in Nigeria
In Nigeria, cardiovascular disease accounts for 9% of all deaths each year [1]. Hypertension is a major driver of cardiovascular disease burden, with a prevalence between 32.5% and 38.1% among adults in Nigeria [2, 3]. However, access to care and treatment for hypertension in Nigeria is inadequate, with only 12.0–33.6% of hypertensive individuals estimated to receive treatment [2, 3]. Moreover, blood pressure control rates are extremely low, ranging from 2.8 to 12.4% [2, 3]. Several factors contribute to this situation, including poor detection and management of hypertension at primary health centers (PHCs), a shortage of health workers (HWs), limited knowledge among some HWs, and inadequate equipment and supplies at health facilities [4].
The Nigerian Federal Ministry of Health (FMOH) has established national targets and developed a roadmap to address the rising burden of non-communicable diseases based on the World Health Organization (WHO) HEARTS hypertension control technical package [5,6,7]. In collaboration with the National Primary Healthcare Development Agency (NPHCDA), WHO, and Resolve to Save Lives, the FMOH launched the Nigerian Hypertension Control Initiative in 2020 [8]. The initiative aims to improve population-level blood pressure control by strengthening and scaling up screening, diagnosis, treatment, monitoring, and health education at the primary health care level.
Nigeria Hypertension Control Initiative strategies include standardizing hypertension treatment with a simple treatment protocol and implementing task shifting and task sharing of hypertension service delivery duties. This approach engages all cadres of PHC staff in hypertension management. The government is currently conducting in-person training of HWs in PHCs across the country using Nigeria-specific guidelines. However, traditional in-person training has several limitations.
Current gaps in health worker training
Low- and middle-income countries face significant challenges in establishing and maintaining a skilled health workforce to combat the growing burden of non-communicable diseases and other health challenges [9]. Conventional HW in-service training methods have not kept up with the rapid evolution of clinical guidelines and best practices [10, 11]. Nigeria has over 30,000 PHCs that are staffed by hundreds of thousands of HWs [12]. Providing in-person training to upskill the entire PHC workforce on new hypertension guidelines would be a costly and logistically challenging endeavor. The system of pre-service HW training is also under strain. Meanwhile, developing countries continue to face severe shortages of HWs, particularly in rural and underserved areas [13].
The COVID-19 pandemic has further highlighted the need for innovative approaches to HW training. The pandemic significantly disrupted traditional training methods like in-person seminars and workshops [14, 15]. Online training is emerging as a viable option to provide health professionals with the flexibility to study at their own pace and from any location while minimizing the risk of the spread of infection [14].
Present study
Our team previously piloted and evaluated a short, mobile-optimized online infection prevention and control course with HWs in Nigeria [15]. We found that the course had high completion rates and strong learning gains. Based on the success of the online infection prevention and control course, we applied a similar methodology to train HWs based in PHCs in Nigeria on new national hypertension diagnosis and management guidelines.
Methods
Program design informed by learning science
We expanded on the learning approach we developed in previous pilots of an infection prevention and control course in Nigeria [15]. We used insights from the learning sciences and our understanding of HWs’ learning and technology needs to develop a set of design principles. These include:
-
Structuring the learning around clinical cases that are directly relevant to HWs’ practice. This approach can boost HWs’ interest and motivation [16]. It also allows HWs to directly apply experiences and knowledge stored in long-term memory.
-
Engaging HWs through continuous low-stakes assessments (quiz questions) with constructive feedback. These assessments are intended to promote learning rather than merely evaluate learners [17]. Each question is accompanied by a brief explanation, which improves learners’ subjective experience [18].
-
Developing modules that repeat and expand upon key concepts, harnessing the benefits of spaced repetition to facilitate learning [19].
-
Focusing on essential content and eliminating nonessential material, which improves factual retention [20].
-
Teaching basic knowledge and skills, which may be more appropriate for online HW training than teaching advanced clinical practices [16].
-
Offering short courses, which increases course completion [21].
-
Implementing a user-friendly and well-organized learning experience, which reduces frustration and maintains learners’ self-efficacy [22].
-
Requiring learners to complete a short “sample” module to enroll in the full course. Some learners who sign up for free online courses do not intend to complete them [23], so this small commitment helps to ensure that those who enroll are invested in the learning.
Evaluation methodology
To assess short-term knowledge gains we used a pre-/post-test design. The 10-question multiple choice test was given once at the beginning of the course, with the same set of questions given again at the end of the course. Questions were presented in the same order each time, with the order of answers randomized. Although the pre-/post-test emphasized the content taught in the course, the pre-/post-test questions were not repeated in other modules of the course. Learners could only take each of these tests once and no minimum score was required on the test to advance in the course. Learners received minimal feedback (they could see the correct answers but there were no explanations given) after submitting their answers. To evaluate learners’ reactions, HWs answered a short survey at the beginning of the last module of the course. This survey included the net promoter score question, “How likely is it that you would recommend this course to a friend or colleague?” The survey also included two 5-point Likert scale questions assessing learners’ enjoyment of the course and its relevance to their work. Learners provided basic demographic data by answering a short survey at the end of the first (sample) module of the course. We based the survey questions (supplementary file 1) on questions we used in previous courses [15], with some additions and refinements to match the context of this course.
Collaborative course development
The development of the course was a collaborative and coordinated process that involved multiple government stakeholders, academic partners, and non-governmental organizations. These entities included the FMOH, NPHCDA, WHO-Nigeria Office, Johns Hopkins University, the University of Abuja Teaching Hospital’s Hypertension Treatment in Nigeria Project team, and Resolve to Save Lives.
The FMOH coordinated the co-creation of course materials aligned with the National Hypertension Treatment Guideline, developed in 2021. Prior to the pilot study, four hypertension program managers from WHO, NPHCDA, the Hypertension Treatment in Nigeria Project, and RTSL, three FMOH policymakers, and four clinical experts reviewed the course to ensure alignment with local guidelines and cultural context. An example module from the course is provided in supplementary file 2. After the content was reviewed, the course was built on our learning management system and quality assurance was conducted by the team at Resolve to Save Lives.
Next, we conducted user testing at a PHC in Abuja to ensure the course’s usability and effectiveness. Four HWs from different cadres took part in the testing, including a medical doctor, a nurse/midwife, a community health extension worker (CHEW), and a pharmacy technician. HWs were selected who had a smartphone, an email account, and access to cellular data or Wi-Fi internet at the testing site. We carried out individual user testing sessions with each HW. Throughout these sessions, we offered an overview and context for the online hypertension course, secured consent from the participants, and clarified the procedure for accessing the course. The HW then received a text message with a link to the course and accessed selected modules on their mobile device. They were encouraged to provide feedback on their progress, including difficulties encountered, observations, and suggestions. The results of user acceptance testing were used to improve the course content and navigation for the subsequent pilot.
Course dissemination
Enrollment in the pilot online training was open from February 13 to April 20, 2023. Learners who enrolled had access through May 4, 2023 to ensure that they had enough time to complete the course. The FMOH, NPHCDA, the Hypertension Treatment in Nigeria Project manager, and state non-communicable disease coordinators distributed the link to the online course to HWs at Nigeria Hypertension Control Initiative facilities, hypertension treatment in Nigeria project facilities, and other facilities implementing hypertension control programs. The link was primarily shared via email and WhatsApp. The target audiences included doctors, nurses, and community health workers at PHCs who care for hypertensive patients. Due to task shifting and task sharing, all of these HW cadres contribute to hypertension diagnosis and management in PHCs in Nigeria.
Technologies used
The course was hosted on the LearnWorlds platform [24]. We optimized LearnWorlds settings to remove any unnecessary buttons or menus, simplify navigation, and maximize readability on mobile devices. Learners were required to answer all questions and move through the course in sequence. LearnWorlds was integrated with another tool, Zapier [25], to automatically enroll learners in the full hypertension course after they completed a sample module. Support requests were handled over email and learners used WhatsApp to support each other informally and contact program staff for support.
Data analyses
All data were downloaded from the LearnWorlds platform in.csv format. To calculate pre-/post-test scores, we gave each question equal weight. The net promoter score question was presented on an 11-point scale from 0 (not at all likely) to 10 (extremely likely). We calculated net promoter score by subtracting the percentage of detractors (6 and below) from the percentage of promoters (9 and 10) [26]. Likert scale questions were numerically coded to compute a mean. All data were analyzed in Microsoft Excel. Paired t tests were used to evaluate learning gains.
Results
Enrollment, completion, and learner demographics
748 users entered the first “sample” module of the course. Of these, 574 completed the sample module to enroll in the full course. 75% of enrolled learners (n = 431) completed the course. The mean pre-test score was 65.4% among learners who completed the course, and 59.6% among learners who did not. Over 99% of enrolled learners reported living in Nigeria, and 75% of them were asked to take the course by a supervisor. 59% of learners reported working in a PHC that was part of an existing hypertension control program in Kano State, Ogun State, or the Federal Capital Territory. The vast majority of learners (89%) reported accessing the course on a smartphone or other mobile device. Almost all learners (98%) reported some work responsibilities related to hypertension diagnosis and management or the administration of hypertension programs (Table 1).
70% of learners reported completing training for at least one clinical role (Junior CHEW, CHEW, community health officer, Nurse, Midwife, or Doctor). 54% of learners reported completing some post-secondary schooling (but not a bachelor’s degree), and 34% reported completing a bachelor’s degree.
Learning gains and completion by health worker cadre and education level
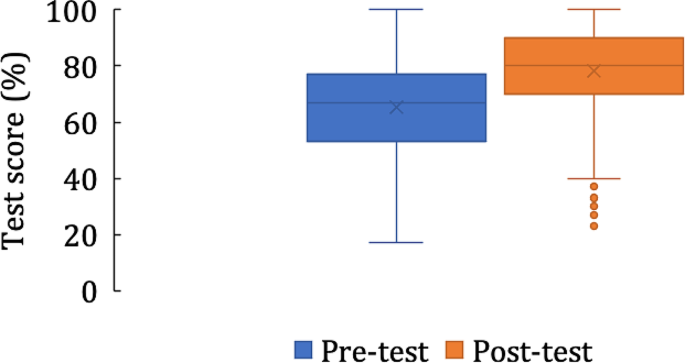
Among the 431 learners who completed the course, the pre-test score was 65.4% and the post-test score was 78.2% (P < 0.001). There was a wide range of scores on both tests (Fig. 1).
There were differences in test scores and course completion by HW cadre (Table 2), but learning gains were significant in all cadres. Nurses, midwives, doctors, and those who completed a bachelor’s degree or above in microbiology or biomedical sciences had the largest learning gains. Doctors had the highest pre-test scores of any group, while community health officers had the lowest pre-test scores. CHEWs had the highest completion percentage and doctors had the lowest completion percentage.
Learning gains interact with study time and prior participation in hypertension control programs
Learners who completed all learning activities spent a median time of 160 min working in the course. Those who took longer to complete the course had greater learning gains than those who spent the median amount of time or less (Table 3). 59% of the 431 learners who completed the course reported working in a PHC that was part of an existing hypertension control program. These learners had higher pre-test scores and lower learning gains than those who were not working at such PHCs (Table 3).
Learner feedback
Of 434 responses to the net promoter score question, the average rating was 9.6/10, corresponding to a net promoter score of + 86. Learners also gave the course high ratings on two Likert-scale questions assessing their enjoyment of the course and its relevance to their work (Table 4).
Discussion
We developed and piloted an online learning approach to train HWs in Nigeria on new national guidelines for hypertension management. The pilot had a high percentage of completion, positive learner feedback, and significant learning gains across different categories of PHC-based HWs. Most importantly, learners significantly gained clinically relevant knowledge regardless of their cadres. Along with our previous work [15], these results suggest that a mobile, digital, on-demand training approach is effective for training PHC-based HWs in Nigeria on best clinical practices in hypertension management. Future research, ideally randomized controlled trials, will be needed to determine the impact of such training on patient care and health outcomes.
This course had a high percentage of completion compared to industry norms, with 75% of enrolled learners completing the course, in contrast to massive open online courses, in which completion rarely exceeds 25% [27,28,29,30]. The high percentage of completion of this course is likely due to its endorsement by the FMOH and the encouragement HWs received to take the course from their supervisors. Factors that affect online course completion include endorsement and promotion by employers, the government, trusted sources, and professional networks [31,32,33]. Other factors reported to promote uptake of online courses include perceived usefulness and value relative to the effort required [29, 34, 35]. We hypothesize that the case-based nature of the training, its brevity, and its focus on only the most relevant material contributed to its effectiveness, as more than 95% of HWs said the course was relevant to their work, and almost all reported performing at least one work task related to hypertension management.
Learning gains were substantial and statistically significant, indicating that HWs’ knowledge of hypertension management improved upon completing the course in all relevant cadres. However, we observed some heterogeneity of learning gains, with HWs who had completed four or more years of post-secondary education (such as nurses, midwives, and medical doctors) having greater learning gains than cadres of HWs with two or three years of post-secondary schooling (CHEWs and community health officers). This association between level of formal schooling and preparedness to succeed in self-paced and self-directed online learning is in keeping with several previous studies, which reported the importance of self-efficacy, motivation, and digital skills to a participant’s success in online learning [33, 36,37,38,39].
HWs who were not staff at PHCs taking part in existing hypertension treatment programs had lower pre-test scores and greater learning gains than those who were. This is at variance with other studies, which suggested that low prior knowledge is associated with poor outcomes in online courses [40,41,42]. It may be that those who were not in existing hypertension programs were more motivated to learn hypertension management, thereby leading to the large knowledge gains we observed in this group. Therefore, this mobile training approach might be useful for introducing HWs to new guidelines while also acting as “refresher training” for HWs who have already learned new guidelines.
Learner feedback was overall positive. Responses to two Likert-scale questions indicated that most learners found the course enjoyable and relevant to their work, with higher ratings than similar questions reported in other courses [43,44,45]. The net promoter score of this course (+ 86) was high, exceeding the “excellent” benchmark of + 50 and the reported net promoter score of other online courses [15, 46, 47].
On-demand, smartphone-based health worker training has the potential to fill the demand for clinical training efficiently and at lower cost compared with traditional, in-person training in Nigeria and other countries. The Nigeria hypertension training course can be deployed to meet several hypertension control program needs: (1) induction training of workers either en masse at facility activation, or when new workers join primary care teams that were previously trained, or (2) refresher training of workers who were already trained.
Online training for HWs is becoming more widespread globally due to higher demand (more HWs who can access digital training) and increasing supply (more options for those learners). The rapid rise in access to cellular internet and increasing smartphone ownership in Africa [48] could be a fulcrum that will promote online training in this part of the world. In Nigeria, an estimated 55% of the population is connected to the internet and over 97% of users access the internet with a mobile device [49]. Most HW cadres that work in PHCs in Nigeria have some post-secondary education, and many have completed bachelor’s degrees, so this group may be among early adopters of technology-enabled learning. It remains unclear whether mobile training applications are best used as an adjunct to traditional in-person group training, or a substitute for in-person training. Finally, rigorous educational and economic evaluations are needed to inform the optimal strategy for primary care health worker training.
Limitations
We only evaluated short-term knowledge gains, and we haven’t yet tested the impact of this training on clinical skills (such as proper blood pressure measurement) or clinical outcomes (such as control of hypertension). Without a comparator group, we can’t be certain that the observed knowledge gains are fully attributable to the online course. All data on learners’ demographics and education levels are self-reported and we did not independently verify the identity of course participants. Many HWs were asked to take the course by their supervisors and were encouraged to complete the course within 14 days, which may have led some HWs to rush through the course to complete it. There was also likely self-selection of HWs with high motivation, access to an internet-connected smartphone, and a certain level of digital literacy and familiarity with navigating through interactive websites.
Conclusions
We found that a simple-to-use, mobile-optimized, case-based online short course can effectively train PHC-based HWs on updated hypertension management guidelines. A high percentage of learners completed the course, learner feedback was very positive, and there were significant learning gains in all cadres of HWs. These results suggest that such training is a scalable way to build health workforce capacity on new clinical guidelines and to refresh knowledge of best clinical practices. Either on its own or in combination with traditional in-person group trainings, this approach could be applied to a variety of topics to improve HWs’ adherence to evidence-based practices in Nigeria and elsewhere.
Data availability
De-identified data are available from the corresponding author upon request.
Abbreviations
- CHEW:
-
community health extension worker
- FMOH:
-
Federal Ministry of Health
- HW:
-
health worker
- NPHCDA:
-
National Primary Health Care Development Agency
- PHC:
-
primary health center
References
World Health Organization. https://ncdportal.org/CountryProfile/GHE110/NGA, ncdportal.org. https://ncdportal.org/CountryProfile/GHE110/NGA (accessed May 21, 2023).
Adeloye D, et al. Prevalence, awareness, treatment, and control of hypertension in Nigeria in 1995 and 2020: a systematic analysis of current evidence. J Clin Hypertens. Feb. 2021;23(5). https://doi.org/10.1111/jch.14220.
Odili AN, et al. Prevalence, awareness, Treatment and Control of Hypertension in Nigeria: data from a Nationwide Survey 2017. Global Heart. Jul. 2020;15(1). https://doi.org/10.5334/gh.848.
Nelson O. Management of hypertension in Nigeria: the barriers and challenges. J Cardiol Cardiovasc Med. Mar. 2021;6(1):023–5. https://doi.org/10.29328/journal.jccm.1001112.
World Health Organization., Hypertension, World Health Organization, Mar. 16, 2023. https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed May 21, 2023).
World Health Organization. HEARTS technical package for cardiovascular disease management in primary health care. World Health Organization; 2020.
Federal Ministry of Health, Nigeria., National Multi-sectoral Action Plan for the Prevention and Control of Non-communicable Diseases (2019–2025), 2019.
Resolve to Save Lives. accessed May 21, Resolve to Save Lives: New program announced to lower high blood pressure in unreached communities across Nigeria, resolvetosavelives.org. (2023). https://resolvetosavelives.org/about/press/new-program-announced-to-lower-high-blood-pressure-in-unreached-communities-across-nigeria
Ganju A, et al. Systemic solutions for addressing non-communicable diseases in low- and Middle-Income Countries. J Multidisciplinary Healthc. Jul. 2020;13:693–707. https://doi.org/10.2147/jmdh.s252300.
Zulu JM, Perry HB. Community health workers at the dawn of a new era. Health Res Policy Syst. Oct. 2021;19. https://doi.org/10.1186/s12961-021-00761-7.
Nicol E, Turawa E, Bonsu G. Pre- and in-service training of health care workers on immunization data management in LMICs: a scoping review. Hum Resour Health. Dec. 2019;17(1). https://doi.org/10.1186/s12960-019-0437-6.
Makinde OA, Azeez A, Bamidele S, Oyemakinde A, Oyediran KA, Wura A et al. Development of a Master Health Facility List in Nigeria. Online J Public Health Inf. 2014;6(2).
Puchalski Ritchie LM, Khan S, Moore JE, Timmings C, van Lettow M, Vogel JP et al. Low- and middle-income countries face many common barriers to implementation of maternal health evidence products. Journal of Clinical Epidemiology [Internet]. 2016 Aug [cited 2020 Jan 15];76:229–37. Available from: https://www.sciencedirect.com/science/article/pii/S0895435616001542.
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A et al. Introduction of Mobile Health Tools to support COVID-19 training and surveillance in Ogun State Nigeria. Front Sustainable Cities. 2021;3.
Thomas MP, Kozikott S, Kamateeka M, Abdu-Aguye R, Agogo E, Bello BG et al. Development of a simple and effective online training for health workers: results from a pilot in Nigeria. BMC Public Health. 2022;22(1). https://doi.org/10.1186/s12889-022-12943-1
Bin Mubayrik HF. Exploring Adult Learners’ Viewpoints and Motivation Regarding Distance Learning in Medical Education. Advances in Medical Education and Practice [Internet]. 2020 Feb 19 [cited 2020 May 25];11:139–46. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7036663/.
Roediger HL, Karpicke JD. The power of testing memory: Basic Research and implications for Educational Practice. Perspect Psychol Sci. 2006;1(3):181–210.
Thomas MP, Türkay S, Parker M. Explanations and interactives improve subjective experiences in Online Courseware. Int Rev Res Open Distrib Learn. 2017;18(7).
Kerfoot BP, Fu Y, Baker H, Connelly D, Ritchey ML, Genega EM. Online Spaced Education generates transfer and improves Long-Term Retention of Diagnostic skills: a Randomized Controlled Trial. J Am Coll Surg. 2010;211(3):331–337e1.
Brame CJ. Effective Educational Videos: Principles and Guidelines for Maximizing Student Learning from Video Content. Perez KE, editor. CBE—Life Sciences Education [Internet]. 2016;15(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5132380/#B35.
Padilla Rodriguez BC, Armellini A, Rodriguez Nieto MC. Learner engagement, retention and success: why size matters in massive open online courses (MOOCs). Open Learning: J Open Distance e-Learning. 2019;1–17.
Simunich B, Robins DB, Kelly V. The impact of Findability on Student Motivation, Self-Efficacy, and perceptions of Online Course Quality. Am J Distance Educ. 2015;29(3):174–85.
Reich J. MOOC Completion and Retention in the Context of Student Intent [Internet]. er.educause.edu. 2014 [cited 2016 Sep 26]. Available from: http://er.educause.edu/articles/2014/12/mooc-completion-and-retention-in-the-context-of-student-intent.
LearnWorlds. Create & Sell Online Courses from Your Own Site. LearnWorldscited. (2023 Jul 26) Available from https://www.learnworlds.com.
Zapier. The easiest way to automate your work. Zapier. Published 2011. (cited. 2023 Jul 26). Available from https://zapier.com/.
Koladycz R, Fernandez G, Gray K, Marriott H. The net promoter score (NPS) for insight into client experiences in sexual and Reproductive Health clinics. Global Health: Sci Pract. 2018;6(3):413–24.
Reich J, Ruipérez-Valiente JA. The MOOC pivot. Science. 2019;363(6423):130–1.
Fu Q, Gao Z, Zhou J, Zheng Y. CLSA: a novel deep learning model for MOOC dropout prediction. Comput Electr Eng. 2021;94:107315.
Gütl C, Rizzardini RH, Chang V, Morales M. Attrition in MOOC: lessons learned from Drop-Out students. Commun Comput Inform Sci. 2014;37–48.
Jordan K. Massive open online course completion rates revisited: Assessment, length and attrition. Int Rev Res Open Distrib Learn. 2015;16(3).
Stark CM, Pope J. Massive Open Online courses: how registered dietitians Use MOOCs for Nutrition Education. J Acad Nutr Dietetics. 2014;114(8):1147–55.
Scott KW, Dushime T, Rusanganwa V, Woskie L, Attebery C, Binagwaho A. Leveraging massive open online courses to expand quality of healthcare education to health practitioners in Rwanda. BMJ Open Qual. 2019;8(4):e000532.
Magaña-Valladares L, Rosas-Magallanes C, Montoya-Rodríguez A, Calvillo-Jacobo G. Celia Mercedes Alpuche-Arande, Sebastián García-Saisó. A MOOC as an immediate strategy to train health personnel in the cholera outbreak in Mexico. BMC Med Educ. 2018;18(1).
Ma L, Lee CS. Investigating the adoption of MOOCs: a technology-user-environment perspective. J Comput Assist Learn. 2018;35(1):89–98.
Ma L, Lee CS. Drivers and barriers to MOOC adoption: perspectives from adopters and non-adopters. Online Information Review. 2020;ahead-of-print(ahead-of-print).
Barnard L, Paton V, Lan W. Online Self-Regulatory Learning behaviors as a Mediator in the relationship between online course perceptions with achievement. Int Rev Res Open Distrib Learn. 2008;9(2).
Lee Y, Choi J, Kim T. Discriminating factors between completers of and dropouts from online learning courses. British Journal of Educational Technology [Internet]. 2012 Apr 20 [cited 2019 May 26];44(2):328–37. Available from: https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1111/j.1467-8535.2012.01306.x.
Prior DD, Mazanov J, Meacheam D, Heaslip G, Hanson J. Attitude, digital literacy and self efficacy: Flow-on effects for online learning behavior. The Internet and Higher Education [Internet]. 2016 Apr [cited 2019 Apr 19];29:91–7. Available from: https://www.sciencedirect.com/science/article/abs/pii/S109675161630001X.
Wang Y, Baker R. Grit and intention: why do Learners Complete MOOCs? Int Rev Res Open Distrib Learn. 2018;19(3).
Kennedy G, Coffrin C, de Barba P, Corrin L. Proceedings of the Fifth International Conference on Learning Analytics And Knowledge New York: Association for Computing Machinery; 2015. Predicting success: how learners’ prior knowledge, skills and activities predict MOOC performance; pp. 136–140.
Butcher KR, Sumner T. How does prior knowledge impact students’ online learning behaviors? Int J Cyber Behav Psychol Learn. 2011;1(4):1–18.
Bingol I, Kursun E, Kayaduman H. Factors for success and course completion in massive Open Online courses through the Lens of participant types. Open Praxis. 2020;12(2):223.
Meijerman I, Nab J, Koster AS. Designing and implementing an inquiry-based undergraduate curriculum in pharmaceutical sciences. Currents Pharm Teach Learn. 2016;8(6):905–19.
Amini H, Gregory ME, Abrams MA, Luna J, Roland M, Sova LN, et al. Feasibility and usability study of a pilot immersive virtual reality-based empathy training for dental providers. J Dent Educ. 2021;85(6):856–65.
Gable BD, Hommema L. In-Situ Simulation in Interdisciplinary Family Practice Improves Response to In-Office Emergencies. Cureus. 2021.
Jolles MW, Vries M, Hollander MH, Dillen J. Prevalence, characteristics, and satisfaction of women with a birth plan in the Netherlands. Birth. 2019;46(4):686–92.
Palmer K, Devers C. An Evaluation of MOOC Success: Net Promoter Scores. Association for the Advancement of Computing in Education (AACE). 2018;1648–53.
Digital Africa.: Technological Transformation for Jobs [Internet]. [cited 2023 May 18]. Available from: https://www.worldbank.org/en/region/afr/publication/digital-africa.
Digital. 2023: Nigeria [Internet]. DataReportal– Global Digital Insights. 2023 [cited 2023 May 18]. Available from: https://datareportal.com/reports/digital-2023-nigeria.
Acknowledgements
We would like to thank all of the health workers who participated in the course and shared their feedback.
Funding
This study was supported by Resolve to Save Lives. Resolve to Save Lives is funded by Bloomberg Philanthropies, the Bill and Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation. This work was supported, in whole or in part, by the Bill & Melinda Gates Foundation grant award #OPP1175906. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission.
Author information
Authors and Affiliations
Contributions
JO, KO, LJA, KM, AEM, EA, and MPT designed the project, contributed to course development, and wrote the paper. MPT and JO analyzed the data. LN, AG, DO, IAO, MA-O, DO, MMT, COE, SL, HB, MTD, and OC contributed to project design and course development. All authors reviewed this manuscript and provided critical feedback.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work was reviewed and given expedited committee approval by the National Health Research Ethics Committee of Nigeria (NHREC/01/01/2007) and determined to be exempt human subjects research by the Resolve to Save Lives Research Committee. All participants provided informed consent to participate in the training. All methods were carried out in accordance with relevant institutional guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Odu, J., Osi, K., Nguyen, L. et al. On-demand mobile hypertension training for primary health care workers in Nigeria: a pilot study. BMC Health Serv Res 24, 444 (2024). https://doi.org/10.1186/s12913-024-10693-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-10693-x